This article is shared with LebTown by content partner Spotlight PA.
By Charlotte Keith of Spotlight PA and Wyatt Massey of Spotlight PA State College
If she had known, Jessica Clark would have skipped her Friday appointment.
But no one had told her yet, so she took another day off work, begged her mother to watch her sons, and set out with her husband, Titus, on the five-hour drive to Hershey.
Jessica normally tried not to get her hopes up, but this time she couldn’t help it. This appointment with a urologist, she thought, was the final hurdle to getting on the waiting list for a kidney transplant. After that, the call could come any time.
At 31, Jessica had lived with kidney failure for almost half her life. She was used to juggling early morning dialysis appointments with her job as a domestic violence counselor and night classes for a degree in psychology. But lately, the balancing act was becoming harder. Hours of dialysis, hooked up to a machine that removes waste from her blood, left her exhausted, with headaches and blurry vision, or too dizzy to stand up. She missed more of her 10-year-old sons’ baseball and soccer games; eventually, Titus told the boys to stop asking her if she would be able to make it.
That Friday morning, May 31, she and Titus told Spotlight PA, the doctor said he’d be in the room during the transplant surgery.
On the long drive back to Erie, Jessica finally let herself feel excited.
The phone rang Monday morning, but it wasn’t the news she had been anticipating. The voice on the other end of the line explained that Penn State Health Milton S. Hershey Medical Center was closing its liver and kidney transplant programs.
The news had been shared with local media outlets the previous week, three days before Jessica’s appointment. But neither she nor Titus remember anyone at Hershey mentioning this during their visit.
After hanging up the phone, Jessica canceled meetings with clients, brushed off a colleague’s concerned questions, and left work without saying why. She didn’t want her sons to see how upset she was, so she got in her car and headed away from the city, across the state line and out past farms and fields, driving for hours so she wouldn’t have to stop and think.
“I didn’t know anything like this could even happen,” she said.
Penn State Health’s decision to suspend, then indefinitely discontinue, kidney and liver transplants after scrutiny from federal regulators plunged Jessica and dozens of other patients into uncertainty. The closure left them to fight against the unforgiving timetable of their declining health as they navigated the financial and logistical challenges of the upheaval in their care.
When a transplant program closes, patients need to be accepted by another hospital before they can receive a donated organ. This isn’t as simple as sending over paperwork: Each transplant program has its own criteria for taking new patients, and the evaluation process can last months. Success isn’t guaranteed.
Due to a shortage of available organs, not everyone receives a transplant in time. Across the country, more than 100,000 people are on the waiting list for a donated organ. Each day, federal statistics show, about 30 people die before receiving a transplant.
Penn State declined multiple interview requests from Spotlight PA to speak with top health system officials for this story. In a statement, a university spokesperson said Penn State understands the “emotional toll” the closure took on patients. “We cannot overstate our sympathy for them at our inability to offer them the treatment they need.”
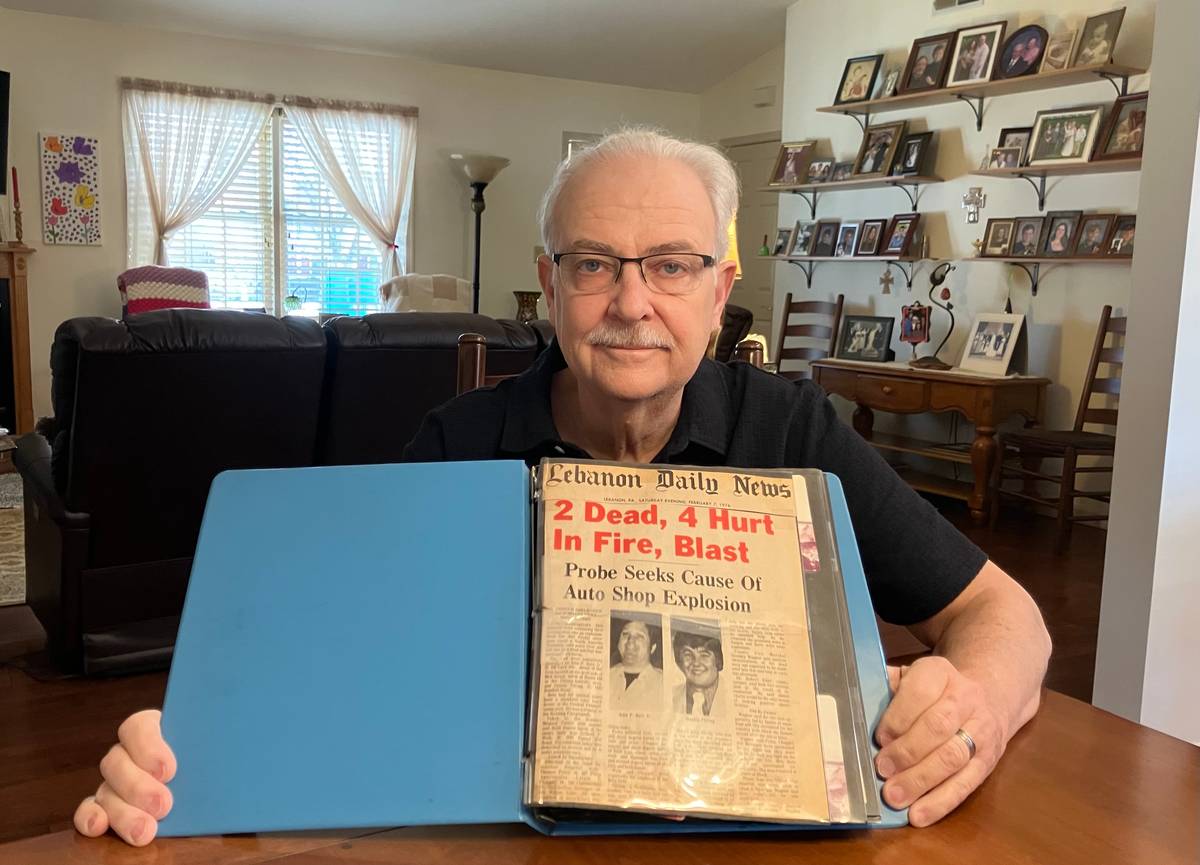
Inside Penn State Health, tensions within the abdominal transplant program had been building for months before the closure. In late 2023, the health system’s director of transplant quality, a surgeon named Raymond Lynch, began raising concerns that the way the program was run cost some patients a chance at a potentially lifesaving organ. Too often, Lynch thought, Hershey patients died while waiting for a liver transplant or became too sick to undergo the procedure. He worried that federal regulators would intervene because so few patients were receiving kidney transplants. And the program’s culture of retaliation made potential problems harder to fix, the surgeon argued.
Lynch raised his concerns with staff members and fellow surgeons, as well as top health system officials including Chief Operating Officer Deborah Addo and Hershey’s Chief Medical Officer Robert Harbaugh, Spotlight PA previously reported. In April, Lynch was abruptly dismissed.
Penn State Health officials have not said what, if anything, was done in response to Lynch’s concerns. Patients told Spotlight PA they had little indication of the internal problems. They trusted the hospital to help them get the transplant they needed.
Penn State Health has pledged to commission a “full and independent review” into why its program failed, but roughly four months later, it has shared few details publicly. In a letter to patients sent in early June, the hospital said only that the decision was made “primarily due to concerns brought to our attention” by a federal regulator.
“This letter was not enough to fix everything,” Jessica said in a video she later posted on Facebook, holding the piece of paper in front of her.
“It was not enough to fix the anxiety. It was not enough to say, ‘Sorry’ — ‘Sorry you used up all your PTO, sorry you used up all that gas money, sorry you used up all that money to stay at hotels near our area.’ This just isn’t enough.”
She crumpled the letter into a ball.
“But maybe tomorrow will be better.”
‘Tremendous community need’
For years, Penn State Health officials have argued that their kidney and liver transplant programs are vital to central Pennsylvania.
Most of the state’s transplant hospitals are clustered around Philadelphia and Pittsburgh. Some urban health systems have clinics in smaller cities and suburbs; these allow patients to have tests done and receive some care, but do not provide the transplant surgery. There are fewer options in rural areas.
At Hershey, quality and safety issues have previously marred the abdominal transplant program. In the spring of 2022, the hospital agreed to stop performing liver and kidney transplants after state and federal investigators uncovered serious safety problems. Later that year, the hospital received an unusually severe public rebuke from a national oversight group.
As the hospital sought to restart transplants, the health system’s CEO at the time, Steve Massini, told regulators that central Pennsylvania residents counted on Hershey to meet the “tremendous community need” for transplant care, according to a confidential summary of the December 2022 meeting obtained by Spotlight PA.
In the same meeting, another senior official said the hospital’s transplant patients, many of whom relied on Medicare and Medicaid, “simply don’t have access to transportation back and forth to other programs.” Fifteen patients waiting for a kidney transplant at that time had declined a referral to another hospital because they didn’t have a way to get there, he said.
The latest failures of the transplant program have forced some patients to travel farther for their care anyway.

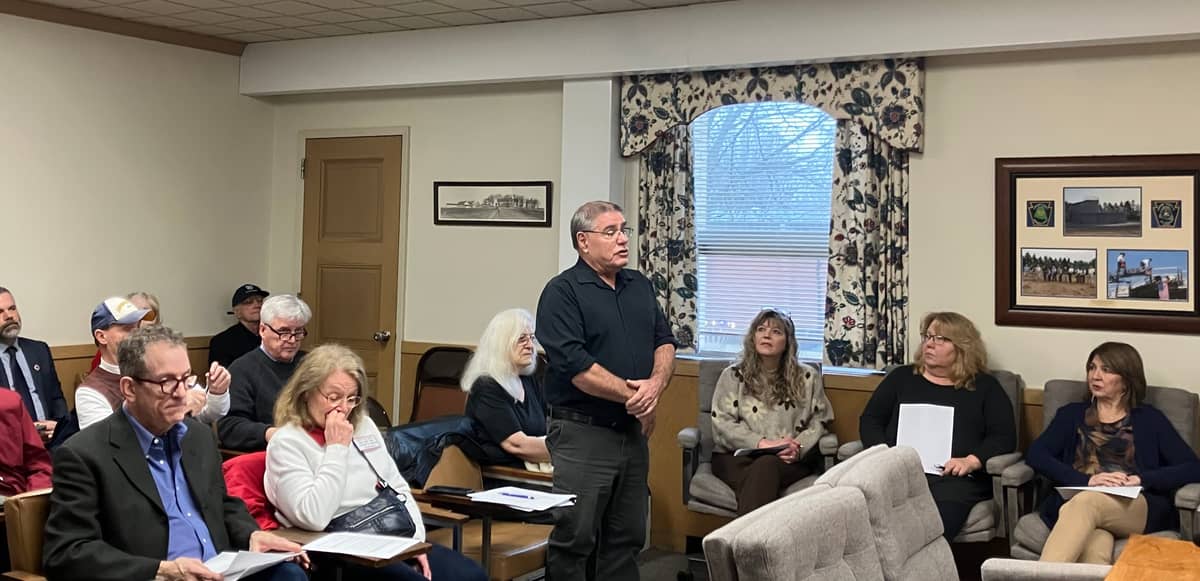
Troy Geiter is one of them. He used to love driving his red Ford Mustang with the top down, but he doesn’t trust himself to get behind the wheel anymore. These days, taking a shower is exhausting. Walking up the stairs wipes him out. Eating makes him nauseous, so he keeps a bucket nearby. The hernia where the incisions were made feels like a basketball in his stomach.
Troy, 47, received a liver transplant at Hershey in 2021. Then came a complicated and arduous recovery: malnutrition, a dangerous infection, and a case of COVID-19 that resulted in pneumonia. Weeks lying in a hospital bed aggravated the pain in his lower back, making it difficult for him to walk, sleep, or sit, medical records note. He lost so much weight that it felt as if there was “no cushion between bone and skin,” he told one doctor.
By late 2023, he was back on the waiting list for a second liver transplant.
After Hershey closed, Troy transferred to Johns Hopkins Hospital in Baltimore. The drive there from his home outside Lancaster takes roughly an hour and a half each way. After about 20 minutes in the car, it feels like someone is tightening a vice in his back, he said. Sometimes, he is so desperate for relief that he lies down horizontally across the backseat. The pain makes him impatient and causes him to snap at his mother or his aunt, who has to take the day off work to drive them to Baltimore. The drive to Hershey was about half as long, and his aunt could take them after her shift.
“I don’t mind doing it, but it’s a lot for me,” said Troy’s aunt, Carol Waltman, who is in her seventies.
Troy could have kept going to Hershey for follow-up appointments from his first transplant. But after the sudden closure, he said, “I started second-guessing everything.” He switched all of his care to Johns Hopkins.
In August, Troy had to spend three weeks in the hospital. His mother and aunt could visit only once a week because of the distance. When Troy had to stay at the hospital in Hershey, they were able to go every other day.

Lost time
In late May, as Penn State Health employees began calling patients about the transplant closure, they were limited in what they could disclose. An outline of talking points obtained by Spotlight PA directed them to tell patients that the hospital made the decision following discussions with a federal regulator and an internal review.
“I’m sorry that I can’t provide further details than that,” the memo instructed employees to say.
Health systems must communicate with different groups — such as patients, employees, oversight bodies, and the public — that each have different needs and expectations, said Glen Nowak, co-director of the Center for Health and Risk Communication at the University of Georgia. Accrediting agencies or regulators can also constrain what a hospital can disclose, he said. In this environment, transparency might not be a major part of the communication process.
In addition to calling, Penn State Health mailed notice of the program’s closure to patients, as required by federal regulators.
“The letter was insulting,” said Niki Burawski, who lives in the Reading area. “It was just very cold, very cold. No apologies. No sorry for the inconvenience.”
Niki was scheduled to give a kidney to her 13-year-old son, Dylan, at Hershey in July. The preschool teacher had burned through her vacation time during the prior school year to undergo the necessary testing. The July date would have allowed Dylan to recover before the start of the fall semester.
The Burawskis chose Hershey for the transplant over the Children’s Hospital of Philadelphia because of its proximity to Dylan’s school. It was also where Dylan was born, and the family had great relationships with its doctors, Niki said. The Burawskis researched why Penn State Health shut down transplants in 2022 and figured the program would be under intense scrutiny, and therefore reliable, she said.
After the closure, the Burawskis transferred to CHOP. Niki and Dylan had to undergo testing again. Trips into Philadelphia took hours and cost hundreds of dollars in tolls, she said.
“There’s not a single day this summer that I didn’t think about how pissed off I am,” Niki told Spotlight PA.
In late August, both Dylan and Niki went back to school without a transplant date.
She blames herself too. If she had initially chosen CHOP, Dylan’s surgery might be done already. She could have used her time off to take her children on a vacation or to visit their grandparents, she said.
Instead, all that time is lost.

Losing hope
Karen Miller’s hospital bag was packed. It wasn’t anything special, just a reusable grocery bag filled with shirts, shorts, and socks, but she wanted to be ready. The kidney transplant she needed wasn’t far away. She was sure of it.
It was April, and Karen was still recovering from a liver transplant at the end of January and multiple stints in the intensive care unit at Hershey Medical Center. Now, at 58, her kidneys were failing too. As she started the evaluation to get on the hospital’s waiting list for a kidney transplant, the road ahead looked so daunting that she sometimes felt like giving up. To encourage her, Karen and her husband Larry recall, one of the doctors had said he wouldn’t be surprised if she had the transplant by July 4.
Karen clung to this date like a liferaft. She started thinking about the weeks and months after the transplant. She and Larry would be able to do normal things again, she told herself. Maybe they could go on vacation; they had always talked about going back to Maine.
Karen had another reason to be optimistic: Because she was a liver transplant recipient and on dialysis, she would get special priority on the kidney waiting list — as long as she was on it by the one-year anniversary of the transplant, a national policy called “safety net priority.” Otherwise, the wait could last years.
By late April, Karen could still walk only short distances, and needed more tests and follow-up appointments. But overall, she seemed a “suitable candidate for kidney transplantation,” one doctor wrote in her medical records. A few weeks later, another doctor noted: “She is excited and is looking forward to kidney transplant possibly in July.”
Behind the scenes, however, Hershey’s abdominal transplant unit was in turmoil, following the abrupt dismissal of Lynch, Penn State Health’s director of transplant quality. Before his departure, Lynch had raised concerns with at least two top administrators about patient safety and the number of organ offers the hospital was turning down, Spotlight PA previously reported.
In letters sent to Penn State Health leaders, one employee argued that Lynch’s departure was “plain retaliation” for his attempts to “objectively review” data and patient outcomes. Leaders blamed Lynch’s departure on financial constraints, another employee wrote, but “no one in our department believes that.”
Karen, meanwhile, continued the evaluation process with another appointment in the third week of May. She had no way of knowing that federal regulators were visiting the hospital that same week to review the kidney and liver transplant programs. Hershey had already agreed to temporarily stop performing liver transplants; by the end of the week, regulators asked the hospital to suspend kidney transplants too. The request came as a “tremendous surprise,” hospital president Don McKenna told staff in a meeting that Friday.
Less than two weeks later, Hershey’s kidney and liver transplant programs closed indefinitely. More than 30 kidney patients had already been co-listed at other hospitals prior to the closure, according to federal data. But more than 60, including Karen, were only listed at Hershey and needed to transfer their care.
This process isn’t always straightforward.
Each hospital has its own criteria for putting patients on the waiting list, so patients from Hershey had to start the extensive evaluation process all over again. This often involves an initial, daylong appointment to meet with surgeons and specialist doctors, and sometimes social workers, financial counselors, and dieticians. Follow-up appointments and additional tests can drag out the wait.
By Oct. 4, four months after the closure, all of Penn State Health’s liver transplant patients had transferred to other hospitals, according to a Penn State Health spokesperson. But more than 40 patients on the hospital’s kidney waitlist were “waiting to be listed at other transplant centers.”
During the evaluation, patients can continue to accrue waiting time, an important factor in how long it takes to be offered a kidney. But they cannot receive a transplant until they are officially listed at a hospital and designated as an “active” candidate. (A patient’s status can be changed to “inactive” if they fall behind on required testing or become too sick to receive a transplant.)
After Hershey’s closure, UPMC’s Harrisburg location received so many referrals for kidney transplant patients that the wait time for an evaluation increased to 10 weeks, a spokesperson said.
The final decision whether to add a patient to the waiting list is usually made by a hospital committee. There’s always the possibility of “no.”
July 4 came and went, but Karen did not unpack her bag. She had an evaluation scheduled the following week at UPMC in Harrisburg. But the hospital declined to put her on its waiting list; in a letter, doctors wrote that she was “too frail.” Karen tore the hospital’s folder of paperwork into pieces and threw them in the trash. The “safety net” began to feel more like a looming deadline.
When the pain in her body became overwhelming, Karen would imagine her funeral. “Losing hope: convinced will die,” read the crisis plan she had developed with a counselor. She had found ways to cope, like counting numbers in her head or focusing on different objects in each room of the house. She could close her eyes and escape to the Maine shoreline, remembering the salty tang in the air and the waves crashing onto the rocks. But after she learned that UPMC wouldn’t take her as a patient, these strategies helped only temporarily.

“All I’ve been doing is crying,” Karen told the counselor in an email a few days later.
It wasn’t just the denial that was hard to accept. It was that word, “frail.”
To Karen, “frail” meant weak, decrepit, falling apart. She had never thought of herself as any of those things. Yes, after more than two months in the hospital, she couldn’t hold a knife properly and sometimes needed Larry to cut up her food. She was still sleeping on a recliner in the living room and washing her hair in the kitchen sink, because she was afraid to climb the stairs when she was home alone.
But “frail” made her angry and that anger pushed her to keep going. That summer, Karen still felt like a stranger in her own body, but she’d done weeks of physical therapy, and kept weights and an exercise ball in the kitchen to use after breakfast. She also drove herself to dialysis, even though she was so tired afterward that she had to take a longer route with fewer turns on the way home.
UPMC recommended she try the University of Pennsylvania Health System, but the outcome of the assessment there was similar — like getting “punched again,” Larry said. Karen took the bag out of the closet and began to unpack it.
In late July, she got a call from Temple Health to ask about scheduling an evaluation. She said it wasn’t the right time. Larry would have to take off work again. She’d get her hopes up. She still needed to get stronger.
“I can’t take another denial this soon,” she told Spotlight PA.
One step forward
After hours of research, Jessica scheduled evaluations at four hospitals. All were hundreds of miles from Erie, but she chose them because of the volume of transplants they perform each year. After what happened at Hershey, she didn’t want to take any chances. “I just want whoever’s going to do it,” she said.
The summer passed in a blur of early mornings and blood tests. After one trip to New York City, Jessica got home around 3 a.m. and went to dialysis three hours later. On another trip, she and Titus drove back from Lancaster through a thunderstorm; another time, they got a flat tire in Philadelphia — on Titus’ birthday.
They drove hundreds of miles hoping not to get pulled over for an expired inspection sticker, which they hadn’t renewed because they needed the money for gas.
On each trip, they stopped at a Sheetz near State College to buy a Beanie Baby. Jessica wasn’t usually sentimental about stuffed animals, but they became a way of keeping track of all the appointments. She logged so many miles that the toys piled up on the back seat. One, a big-eared elephant, was starting to fade where she had used him as a pillow.
The years Jessica had spent on dialysis might allow her, once she was listed, to receive a donated kidney in a matter of days, one doctor told her. But getting to that point could still take months. At one hospital, the next available appointments with some of the specialists she needed to see were in early 2025, she said.
Then, in late August, a letter arrived from Jefferson Einstein Philadelphia Hospital saying Jessica had been added to their waiting list. She and Titus framed it and hung it on the wall. Jessica had never wanted the boys to know how sick she was, but she started to explain.
“Our next trip to Philadelphia,” she wrote on Facebook, “will be for a kidney!”
But then, another setback emerged. Jessica was on the waiting list, but it wasn’t the step forward she had hoped for. She wouldn’t be eligible to actually receive a donated kidney without more tests — which meant more scheduling, more driving, more weeks in limbo.
She resigned herself to the uncertainty.
WHILE YOU’RE HERE… If you learned something from this story, pay it forward and become a member of Spotlight PA so someone else can in the future at spotlightpa.org/donate. Spotlight PA is funded by foundations and readers like you who are committed to accountability journalism that gets results.