This article is shared with LebTown by content partner Spotlight PA.
By Ed Mahon of Spotlight PA
HARRISBURG — Some Pennsylvania cannabis companies are using incomplete or misleading claims to promote marijuana as a treatment for opioid addiction, potentially putting patients’ lives at greater risk, a Spotlight PA investigation has found.
In a first-of-its-kind review, Spotlight PA examined more than 60 websites offering services in Pennsylvania and consulted numerous health policy experts about the validity of the claims. In some instances where medical research was cited on a website or by a company official, the news organization directly contacted study authors.
The investigation found a wide range of misleading tactics: cherry-picking and misrepresenting parts of studies, making broad claims without citing any specific research, and providing incomplete information about what it takes to qualify for the state’s medical marijuana program.
About half the websites promoted cannabis dispensaries, while the other half were for physicians or companies that help certify patients.
The most alarming examples, according to several of the experts, were online statements made by two companies that help patients become certified to buy medical marijuana at state dispensaries.
Without citing specific evidence, webpages for Releaf Specialists and Compassionate Certification Centers used identical language to claim research suggests medical marijuana can be a “viable substitute” for buprenorphine, one of three drugs approved by the federal government to treat opioid use disorder.
Several health policy experts, cannabis researchers, and medical providers told Spotlight PA the claim was inaccurate, misleading, or possibly dangerous.
Officials with both companies defended the language in response to questions from Spotlight PA. But research provided by each company did not substantiate their claims as they suggested, and some of the authors of those journal articles strongly pushed back on the characterization of their work.
New York addiction psychiatrist Adam Bisaga, an author of one of the scientific articles cited, warned of the risk of using marijuana instead of one of the federally approved opioid use disorder drugs, saying in an email that “advocating substituting cannabis for buprenorphine, methadone, or naltrexone is not based on any research and it may be dangerous.”
The situation exemplifies the confusion and mixed messages patients receive in Pennsylvania, a state with one of the highest fatal drug overdose rates in the country and one of the few to specifically endorse cannabis as a treatment option for people with opioid use disorder.
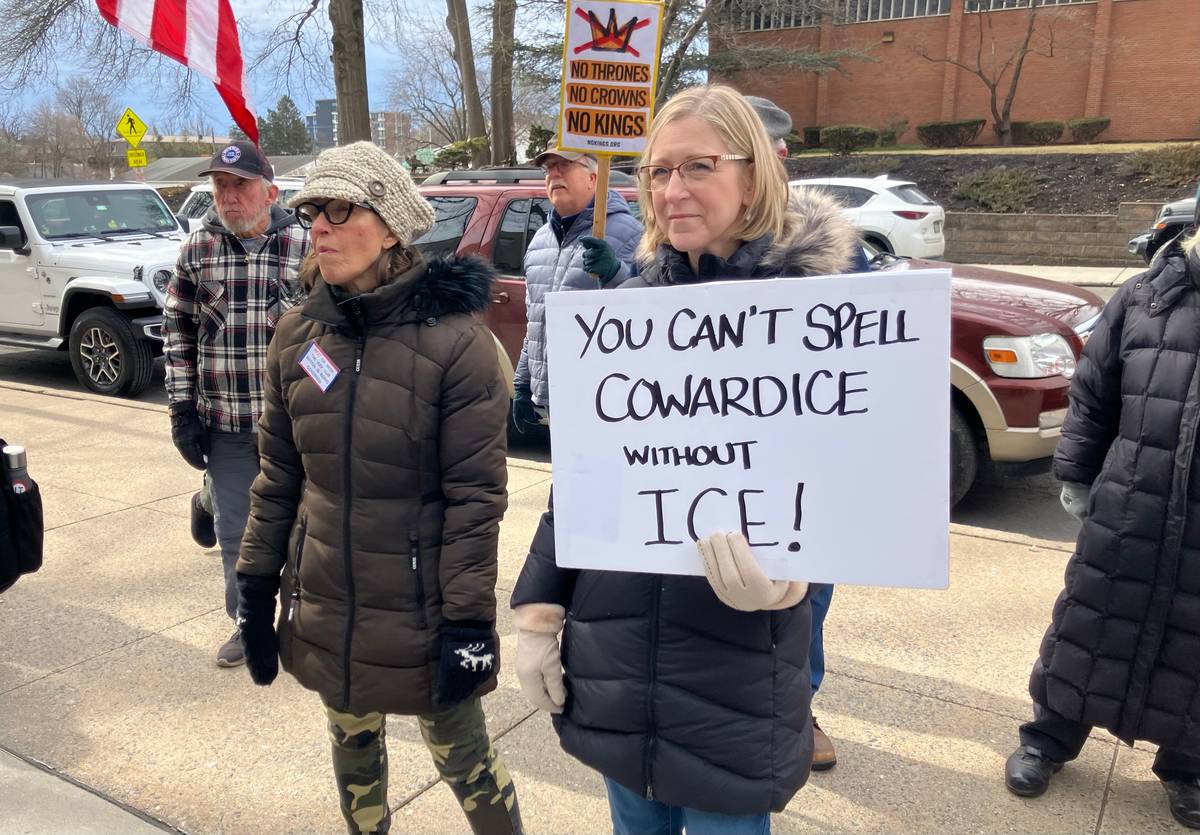
Despite Pennsylvania’s outlier status and the high stakes for people seeking treatment, state regulators do little to ensure cannabis dispensaries make accurate medical claims on their own websites, thousands of pages of records obtained through Right-to-Know requests show.

And while the state’s 2016 medical marijuana law requires the Department of Health to restrict the advertising and marketing of cannabis, it does not specifically mention the certification companies that often play a crucial role in connecting patients with physicians. A department spokesperson said the agency doesn’t “have any regulatory authority” over those companies.
Chelsea L. Shover, an epidemiologist and assistant professor-in-residence at the David Geffen School of Medicine at UCLA, said promoting cannabis as a substitute for buprenorphine as an opioid use disorder treatment is “really dangerous.”
“That’s complete nonsense. If it were up to me, you wouldn’t be allowed to make claims like that,” said Shover, who has studied state cannabis policies and unsupported medical claims made by dispensaries, after reviewing Spotlight PA’s findings. “That’s kind of the worst-case scenario of this advertising.”
Shover was far from the only expert alarmed to see cannabis companies in Pennsylvania making this claim. People with opioid use disorder are about 50% less likely to die when they are treated long-term with buprenorphine or methadone, a major national consensus study found in 2019. No such proof exists for cannabis.
“That’s terrible,” said Erin Zerbo, an addiction psychiatrist in New Jersey and an associate professor at Rutgers New Jersey Medical School, as she reviewed Spotlight PA’s findings. “‘A viable substitute?’ No, that’s bad.”
Among the other findings of Spotlight PA’s investigation:
- Seven websites cited a 2014 study that found medical marijuana laws were associated with lower rates of fatal opioid overdoses. But they ignored a later study that showed the trend didn’t hold up over time and, in fact, reversed. (One dispensary website removed such a reference after Spotlight PA contacted it in December.)
- Seven promoted the benefits of the cannabis compound CBD for opioid addiction treatment, including to help with withdrawal or reduce cravings. But multiple experts told Spotlight PA that at least some of the messages went beyond what research supports.
- The Wolf administration says opioid use disorder should only be a qualifying condition for medical marijuana in certain circumstances, such as when conventional treatments are ineffective, but at least 13 websites didn’t include those caveats when they described what it takes for addiction patients to qualify for cannabis.
“The findings reveal a somewhat deceptive strategy — whether intentional or not — adopted by many dispensaries and cannabis certification websites where very specific and limited scientific research is often cited to support very broad statements about cannabis’ benefits,” Stephanie Lake, a postdoctoral fellow at the UCLA Cannabis Research Initiative, said in an email. “The result of this strategy is an oversimplified and scientifically inaccurate message about cannabis.”
Keith Humphreys, an addiction researcher and professor at Stanford University School of Medicine, said medical cannabis companies should be held to a higher standard than nonmedical businesses.
“Almost everything in here is, if not a lie, pushing the border of truth,” Humphreys said after reviewing Spotlight PA’s findings and examples.
Limited oversight, potential consequences
When Pennsylvania lawmakers legalized medical cannabis in 2016, they put safeguards in place for the messages patients receive. But those have significant limits.
The Pennsylvania Department of Health has the authority to approve or reject advertising, promotional, and marketing materials from cannabis dispensaries, growers, and processors.
But the department rarely uses its power to ensure those companies make accurate medical claims on their websites and social media, according to records obtained through the state’s Right-to-Know law dating back to the start of the program.
When the agency did take enforcement action, the issue often was whether medical marijuana dispensaries failed to follow the required approval process for submitting advertising and marketing materials to the Department of Health, or whether they made references to recreational use.
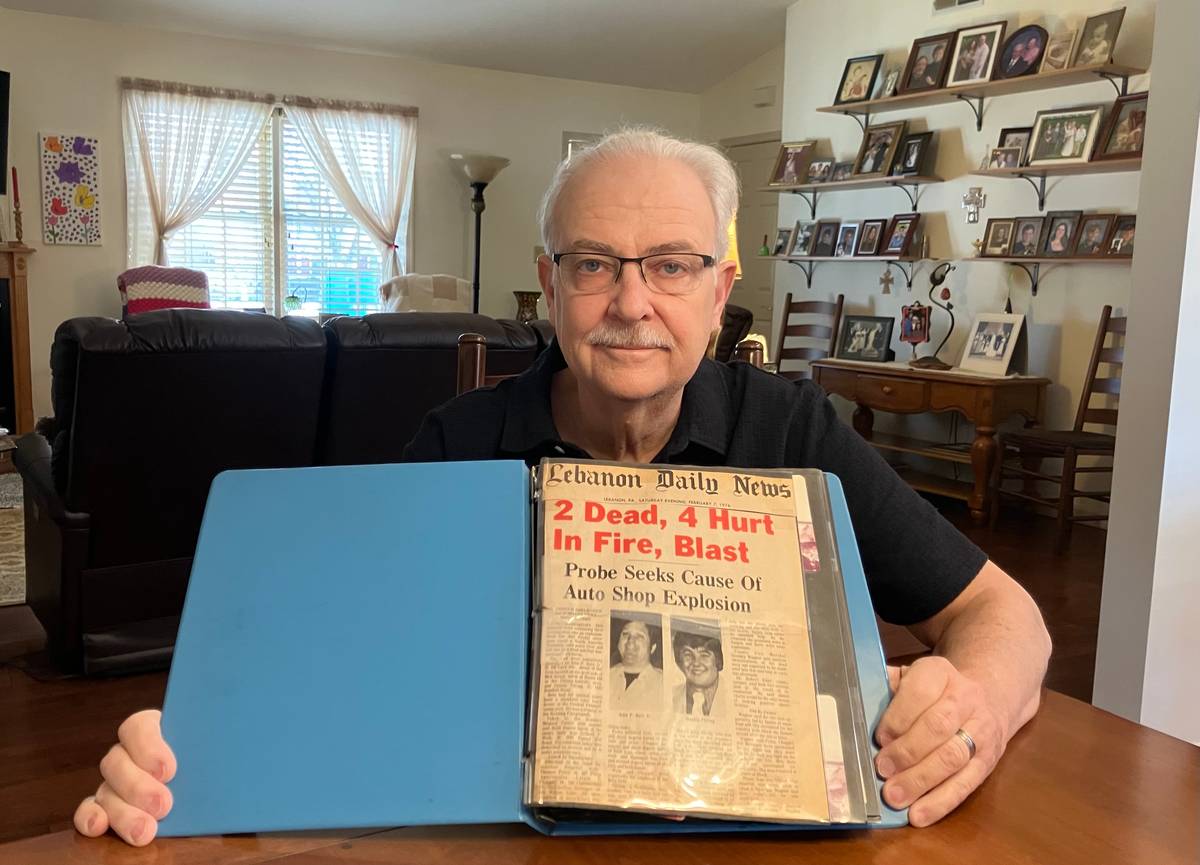
Brendan Saloner, an associate professor at Johns Hopkins Bloomberg School of Public Health, is an author of a 2014 study that found medical marijuana laws were associated with lower rates of fatal opioid overdoses. That research has been cited by dispensaries and certification companies in misleading ways.
Saloner said Spotlight PA’s findings were “definitely consistent with the need for more oversight.”
“There’s a need to communicate with consumers in a consistent way that when dispensaries or other marijuana retailers are making claims that those claims should be vetted for accuracy,” he said.
Health department spokesperson Maggi Barton said the agency “continues to work with medical marijuana dispensaries to ensure they are providing high quality services to Pennsylvanians for all approved medical conditions.” Barton also suggested, in some cases, the department didn’t have enough staff to keep up with the amount of promotional and marketing materials.
Barton said the department does not have enforcement power over cannabis certification companies like Releaf Specialists and Compassionate Certification Centers, which connect people to doctors who make consequential treatment decisions.
‘False hope’
Releaf Specialists described itself online as “an industry leader,” while Compassionate Certification Centers’ website promoted “PA’s Most Trusted Medical Marijuana Certification Providers.”
In sections of their websites focused on opioid addiction, each displayed identical statements: “Research suggests that medical marijuana can be a viable substitute for opioids such as buprenorphine and other prescription drugs.” Neither webpage included a link to said research.
Releaf Specialists owner Bob Scherer, who’s not a physician, suggested the website language was provided by a third-party contractor that he declined to name. He defended the statement, saying it’s “broad and generalized enough that it allows patients to discover and do more research about how cannabis can help them” with opioid addiction.
“I’m just saying that, based off of the state guidelines, and if patients have not had positive outcomes with traditional therapies, then cannabis could be a viable means for them, and they have the option in the state of Pennsylvania to try it,” he said.
Scherer later shared two medical science journal articles with Spotlight PA to support the claim.
One of them was an article co-authored by Bisaga, the New York addiction psychiatrist who told Spotlight PA he was concerned about the possibility of people with opioid use disorder using cannabis as a substitute for federally approved medication.
The other journal article Scherer shared was a review of existing research, and it included context and notes of caution that Releaf Specialists’ webpage did not. In a section titled “Shortcomings of Cannabis in Medication-Assisted Therapy,” the authors wrote there was conflicting evidence for the effectiveness of cannabis for “treatment for opioid misuse.”
Beth Wiese, a neuroscience doctoral candidate at the University of Arizona and an author of the article, said she supports having opioid use disorder as a qualifying condition for cannabis but she still sounded a note of caution.
“I don’t know that we are there to call it a substitute yet,” Wiese said. “Some individuals may find that it works better for them as a substitute. But other people, it may not. I just don’t think we’re there to know exactly.”
Compassionate Certification Centers leaders also defended the language and shared two medical science journal articles in defense, neither of which claimed medical marijuana can be a viable substitute for buprenorphine.
Chief Executive Officer Melonie Kotchey — who has an MBA in health-care administration and medical billing and coding, according to the company’s website — also referred Spotlight PA to a report on the company’s website. Kotchey didn’t specify which report, but her description matched one dated December 2019 that was based on a patient survey the company helped develop.
That report did not compare outcomes for patients who use cannabis instead of buprenorphine, which is not mentioned at all. It also lumped together several conditions, saying 99.62% of patients surveyed “were able to reduce pain, better sleep, less anxiety, less seizures, appetite increase, less vomiting, nausea, addiction withdrawal symptoms, decrease with muscle spasms, improved energy and less seizures.”
Bradford Buege, a physician who the company website describes as board-certified in family practice and emergency medicine, did not cite any studies in an email to Spotlight PA. “My [patients’] input is and always will be valued more above all else,” Buege wrote. “[D]on’t contact me again w your pharmaceutical bs.”
Jennifer Hawks, the company’s chief medical director, took the argument in favor of cannabis over buprenorphine further than the webpage, saying in an email that cannabis and the cannabis compound CBD “are much less invasive and much safer than buprenorphine by far.” A 2019 report from the National Academies of Sciences, Engineering, and Medicine said buprenorphine and other federally approved medications for opioid use disorder “are safe and highly effective.”
Hawks is a licensed naturopathic doctor in Arizona, a state where those practitioners can certify patients for cannabis. That is not the case in Pennsylvania, according to the Wolf administration.

Hawks cited two medical science journal articles, but neither examined addiction treatment outcomes for people who used medical marijuana versus buprenorphine.
Matisyahu Shulman, an addiction psychiatrist in New York and an author of one of the articles, told Spotlight PA that the point of a section Hawks cited is that people should use buprenorphine as a long-term treatment, not for just a week or two weeks. The article, an overview of research on buprenorphine, didn’t mention cannabis or CBD.
Shulman told Spotlight PA “buprenorphine saves lives,” and he said using anything other than a federally approved medication for opioid use disorder is “pretty dangerous.”
Neuroscientist Yasmin Hurd, a leading CBD researcher and an author of the second article Hawks cited, called Compassionate Certification Centers’ online statements about cannabis and opioid use disorder “blatantly incorrect” and “beyond misleading.”
“They’re giving false hope,” Hurd told Spotlight PA.
Hurd, director of the Addiction Institute at the Icahn School of Medicine at Mount Sinai, hopes the cannabis compound CBD will one day become a federally approved medication for opioid use disorder.
She and her colleagues have found CBD can reduce cue-induced craving and anxiety for people who have a history of heroin use, but she said those were smaller studies that lay the groundwork for more research. A 2019 study by Hurd and fellow researchers, for instance, examined 42 patients over 10 days, and her team said long-duration treatment studies were needed.
And she told Spotlight PA it’s important to distinguish between CBD, which is one compound of cannabis, and medical marijuana, which includes many compounds that can have different effects. They aren’t interchangeable, Hurd said.
“We should hold people accountable, especially today, to be very clear about what is it that they are promoting and really substantiate that,” Hurd said.
‘A lot of optimism’ but little evidence
When Pennsylvania added opioid use disorder as a qualifying condition for medical marijuana in 2018, the Wolf administration said it was the first state to take such an action.
An April report from that year written by the state’s Medical Marijuana Advisory Board cleared the way for the change, but did not cite any specific research to support it. Instead, the report said cannabis had “been reported by patients to ease the symptoms and process of opioid withdrawal. It has been used by patients as an ‘exit drug’ to get off of heroin and other opiates.”
Multiple health policy experts told Spotlight PA that some people might have success using cannabis as a substitute for other drugs. But they said there are limits to relying on individual stories and anecdotes for creating broad policy or guidelines on how to treat patients — especially when there is good evidence behind other treatments.
“The way my field works is you can’t go from, ‘Well, one person can do it’ to ‘This should be a treatment for 1,000 people,’’ said M-J Milloy, an epidemiologist and research scientist at the British Columbia Centre on Substance Use in Canada. “There’s a lot of optimism around cannabis being a substitute for these sorts of things. But we’re not there yet in terms of what has been proven through controlled trials and other high-quality scientific studies.”

The state’s health secretary at the time, physician Rachel Levine, also didn’t cite any specific research when she formally added opioid use disorder as a qualifying condition. Levine said opioid use disorder should only be a qualifying condition in certain circumstances: when conventional therapies are contraindicated or ineffective, or if cannabis is used alongside another primary therapy.
“It’s important to note that medical marijuana is not a substitute for proven treatments for opioid-use disorder,” Levine, who now serves in President Joe Biden’s administration, said in a news release at the time.
Pennsylvania’s regulations allow any of its authorized cannabis doctors to certify for opioid use disorder. At a Medical Marijuana Advisory Board meeting in May 2019, pediatric neurologist William Trescher raised concerns about the practice, saying he didn’t know how many of those physicians were “true experts” in addiction.
“They can say the person has it,” Trescher, a board member at the time, said according to a meeting transcript. “But I don’t know if they’re going to know how to manage it.”
Neighboring New York has created a higher bar. In order to approve cannabis for opioid use disorder there, practitioners must also have a federal waiver to dispense and prescribe buprenorphine.
The requirement helps ensure these practitioners have some experience treating patients with a substance use disorder, Freeman Klopott, a spokesperson for the state’s Office of Cannabis Management, told Spotlight PA.
Deepika Slawek, a New York physician, co-authored new clinical guidelines for practitioners in that state’s medical cannabis program. The authors said if there is a role for medical cannabis to manage opioid use disorder, “it will be to augment rather than replace” buprenorphine or methadone.
“[E]vidence to support taking medical cannabis to treat opioid use disorder (OUD) is scant,” the authors wrote. “Randomized controlled clinical trials are needed to understand the relationship between medical cannabis use and opioid-related outcomes.”
By limiting who can approve cannabis to treat addiction, Slawek said she hopes those providers are “likely offering buprenorphine first and foremost.”
But the requirement highlights a serious problem: Slawek says there are already too many federal restrictions on which practitioners can prescribe buprenorphine. That creates significant barriers for patients.
The American Society of Addiction Medicine tells practitioners not to recommend cannabis for the treatment of opioid use disorder. Zerbo, the addiction psychiatrist in New Jersey, has a nuanced view.
She believes cannabis can help some patients with opioid use disorder if they use it in addition to a primary treatment. But she said providers “have to be very careful to explain to everyone that it is not” a replacement for the federally approved drugs.
“If we don’t put people on medication, the relapse rate is so high, and people lose their tolerance,” Zerbo said. “And they’re so much more likely to die.”
WHILE YOU’RE HERE… If you learned something from this story, pay it forward and become a member of Spotlight PA so someone else can in the future at spotlightpa.org/donate. Spotlight PA is funded by foundations and readers like you who are committed to accountability journalism that gets results.