This article is shared with LebTown by content partner Spotlight PA.
By Stephen Caruso of Spotlight PA
HARRISBURG — Chronically ill patients could find it easier to get their insurance companies to OK new treatments under a bill Pennsylvania lawmakers are hustling to pass in the final days of the legislative session.
The 67-page bill, which mostly applies to private insurers, would remove prior authorization for emergency care, standardize timelines for insurers to approve or deny a request for treatment, and guarantee that doctors can request that plans cover medications without a patient first trying a cheaper drug.
Supporters say the bill will allow medical providers to spend more time on care rather than fighting with insurance companies, and give patients more clarity and flexibility when deciding on their treatment options.
But changes to a topic as complicated as state insurance law, even when a bill has bipartisan backing, can get messy quick — and threading the needle among a number of well-heeled lobbies has kept similar changes from passing for more than a decade.
Industry groups for insurers, hospitals, and doctors all have a strong lobbying presence in the Capitol. The Insurance Federation of Pennsylvania in particular spends millions of dollars every year to influence legislators.
“It’s a big bill. Details count,” said Sam Marshall, CEO of the federation. He did not specify what concerns he had with the bill, but said that “all sides are working together in good faith.”
The bill has the backing of over 70 condition-specific organizations, including those representing diabetes, arthritis, and multiple sclerosis patients, among other chronic ailments. They argue that the bill will provide patients with quicker access to health care.
At the core of the proposal is an effort to change two key components of the American health care system — prior authorization and step therapy.
Prior authorization empowers an insurance company to decide whether a medical procedure or treatment is medically necessary before it decides to cover it. Step therapy is a specific form of prior authorization for medications, in which an insurer, as a cost-saving measure, asks a patient to try one medication and see proof it isn’t working before they approve the patient’s preferred treatment.
The bill would not completely eliminate either practice. It would instead require insurers to offer exemptions for both, and create a standardized process for doctors to apply for approval or request an exemption, and for patients to appeal an insurance company’s decision.
It would do so by creating standardized electronic forms to apply for approval, setting a statutory timeline for responding to requests (72 hours for urgent requests and 14 days for nonemergency services), requiring written notice from insurers explaining the denial, and giving the state Insurance Department the ability to review the decision.
The bill would also allow physicians to dispute an insurer’s decision directly with a doctor employed by the insurer — a process known as peer-to-peer review — rather than someone who may not have a medical degree.
All told, this “creates a new and more effective process for prior authorization of medical services, and it keeps everything consistent and transparent, from start to finish,” said Sen. Kristin Phillips-Hill (R., York), the bill’s sponsor.
Private insurers defend their review powers as a necessary cost control method to keep insurance rates down. But advocates for patients and providers argue these administrative steps favor insurance companies and diminish their ability to make important health care decisions.
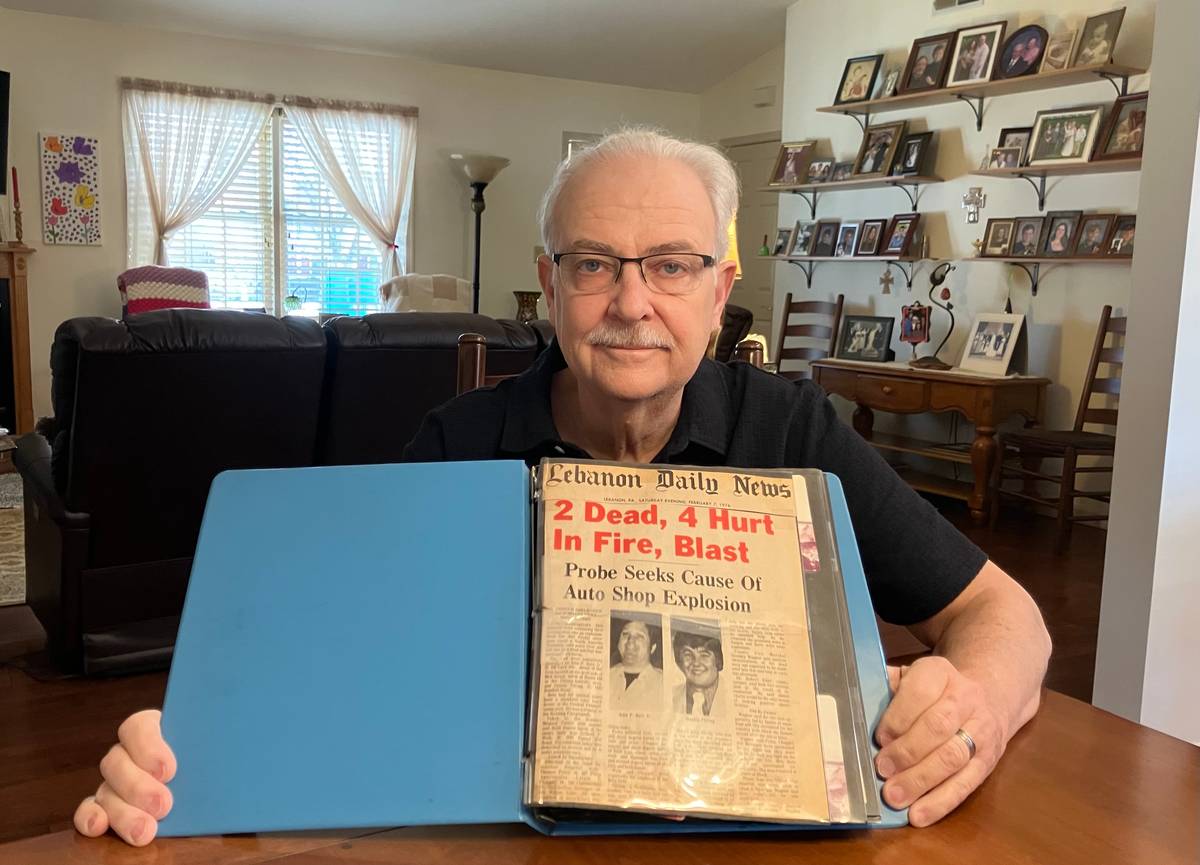
“It would be like having a pipe burst in your home, and being told that you can’t call a plumber and try to mop first,” Mark Lopatin, a retired rheumatologist from outside Philadelphia, told Spotlight PA. Lopatin is on the board of the Pennsylvania Medical Society, which supports the bill.
He’s seen patients who changed insurance providers and were asked to go off a drug they took for years because the new plan wouldn’t cover their medication until they tried a cheaper alternative. The bill would specifically allow for an exemption to step therapy in such a situation.
Lopatin’s experience is not unique. A 2021 American Medical Society survey of 1,000 physicians nationwide reported 93% encountered care delays due to prior authorization, and 82% said those delays have led to patients abandoning treatment.
“Scientific breakthroughs [and] medical advancements mean that in many cases, a diagnosis can now be managed and treated,” said Emma Watson, the chief lobbyist for the state branch of the American Cancer Society and the point person for the other patient groups. “Patients need the ability to quickly assess their condition with their medical professionals to find the best course of action for their individual health needs.”
In some cases, the bill would only bring state insurance law, last rewritten in 1998, in line with federal law. The proposed ban on prior authorization for emergency care, for instance, matches a federal law passed in late 2020. However, medical providers have since challenged that law in court.
Changes to the state insurance law have been considered for years, but have never reached the governor’s desk.
The current proposal passed the Republican-controlled state Senate unanimously in June, but “once it hit the House, there were a lot of people who had concerns,” House Insurance Committee Chair Tina Pickett (R., Susquehanna) said recently.
Her committee approved an amendment on Sept. 20 that kept many key provisions in place. Watson of the patient coalition still backs the bill; Marshall of the insurance federation said he is still reviewing the changes.
Pickett said she anticipates more conversations with stakeholders before the bill can come up for a final vote.
Both Gov. Tom Wolf, a Democrat, and House Speaker Bryan Cutler (R., Lancaster) have voiced interest in seeing through changes to prior authorization in the waning days of the two-year session.
In an email, Wolf spokesperson Beth Rementer said that ensuring that patients receive medical services in a timely manner is a “critical component to ensuring patient access to quality health care,” and that concern is central in talks on the bill.
The bill now awaits a floor vote in the state House, and the state Senate must approve the changes before the measure can make it to Wolf’s desk.
The House has three session days left before the end of the year; the Senate, which must approve the lower chamber’s edits, has six.
WHILE YOU’RE HERE… If you learned something from this story, pay it forward and become a member of Spotlight PA so someone else can in the future at spotlightpa.org/donate. Spotlight PA is funded by foundations and readers like you who are committed to accountability journalism that gets results.