This article is shared with LebTown by content partner Spotlight PA.
By Ashad Hajela of Spotlight PA State College
STATE COLLEGE — In one Pennsylvania county, the coroner’s office relies on an autopsy facility with rusted equipment that does not meet federal workplace standards. The contracted forensic pathologists there perform more than 325 autopsies a year.
A coroner in another county claimed his part-time deputies don’t really investigate deaths. Instead, “they just pick up the body and use this as an opportunity to steer business to their funeral home.”
And only five of Pennsylvania’s 67 counties have accredited coroner or medical examiner offices, which the state doesn’t require but “is perceived as validation of best medicolegal death investigation practices,” according to a new Center for Rural Pennsylvania study.
The August report by the state agency determined that Pennsylvania’s county coroners and medical examiners — the people who investigate suspicious deaths and suss out foul play — lack adequate funding, transparency, and training.
In Pennsylvania, most coroners are elected, and subject to only two requirements: be at least 18 years old and reside in a county for at least a year. Coroners investigate and rule on deaths, initiate autopsies, complete death certificates, and report information vital to legal, public health, and public safety issues. Their work assists law enforcement investigations and helps families get closure when a loved one dies.
The decentralized system allows each coroner to run their office differently, the report found. In practice that causes the accessibility of death data, accreditation, and training — as well as policies and procedures — to vary drastically between municipalities. In short, where you die determines the quality of how your death gets investigated.
In rural counties, challenges are exacerbated because many coroners don’t have access to the labs and specialists who help investigate deaths, researchers said. Meanwhile, they bear the burden of additional costs of transportation and lack of personnel because of their location. They are also less likely to have the accreditation and training that coroners in urban areas do, the study states.
Coroners’ offices act independently from other county entities, but county commissioners determine a large portion of their funding. Plus, the state legislature has limited the funding coroners’ offices receive from cremation authorization permits and death certificates.
Rising costs and fees for death certificates have decreased statewide orders of them, further affecting funding for coroners. A dollar from each death certificate order — which cost $20, plus $10 for online purchases — goes to coroners’ offices, but the remaining $19 gets split between the state’s health department and general fund.
The researchers argue that the legislature should increase the amount coroners’ offices receive per death certificate from $1 to $5, and raise the cap on cremation authorization permits from $50 to $100. The study also recommends that lawmakers standardize coroner salaries.
When a person dies of natural causes, a doctor can certify their death. But if any other cause of death is suspected, the death gets investigated. In Pennsylvania, elected coroners investigate deaths in all counties but Allegheny, Delaware, and Philadelphia, which appoint medical examiners, and Luzerne and Northampton, which appoint coroners.
Public health experts have long debated whether coroners should be elected.
Elected coroners work independently from counties, so they don’t have to fall in line with what a district attorney or county commissioners want them to say, said Christina VandePol, a former elected coroner in Chester County and one of the study’s authors. This autonomy can be important for investigating deaths like those in county jails. VandePol explained that because of her office’s independence, she was able to release the names of nursing homes that had more COVID-19 deaths while she was under pressure not to.
Public health experts who oppose elected corners note that voters might choose unqualified candidates. Hired coroners and medical examiners, they point out, do not have to meet the residence requirements, which allows counties to attract applicants beyond the county’s boundaries.
The study also found the death investigation system lacks transparency and may not be providing county-level death data to the public in a timely or reliable way. On top of that, a state law passed in 2008 requires autopsy records be kept confidential to protect the privacy of the deceased. This prevents residents and journalists from accessing information that could be used to hold coroners’ offices accountable.
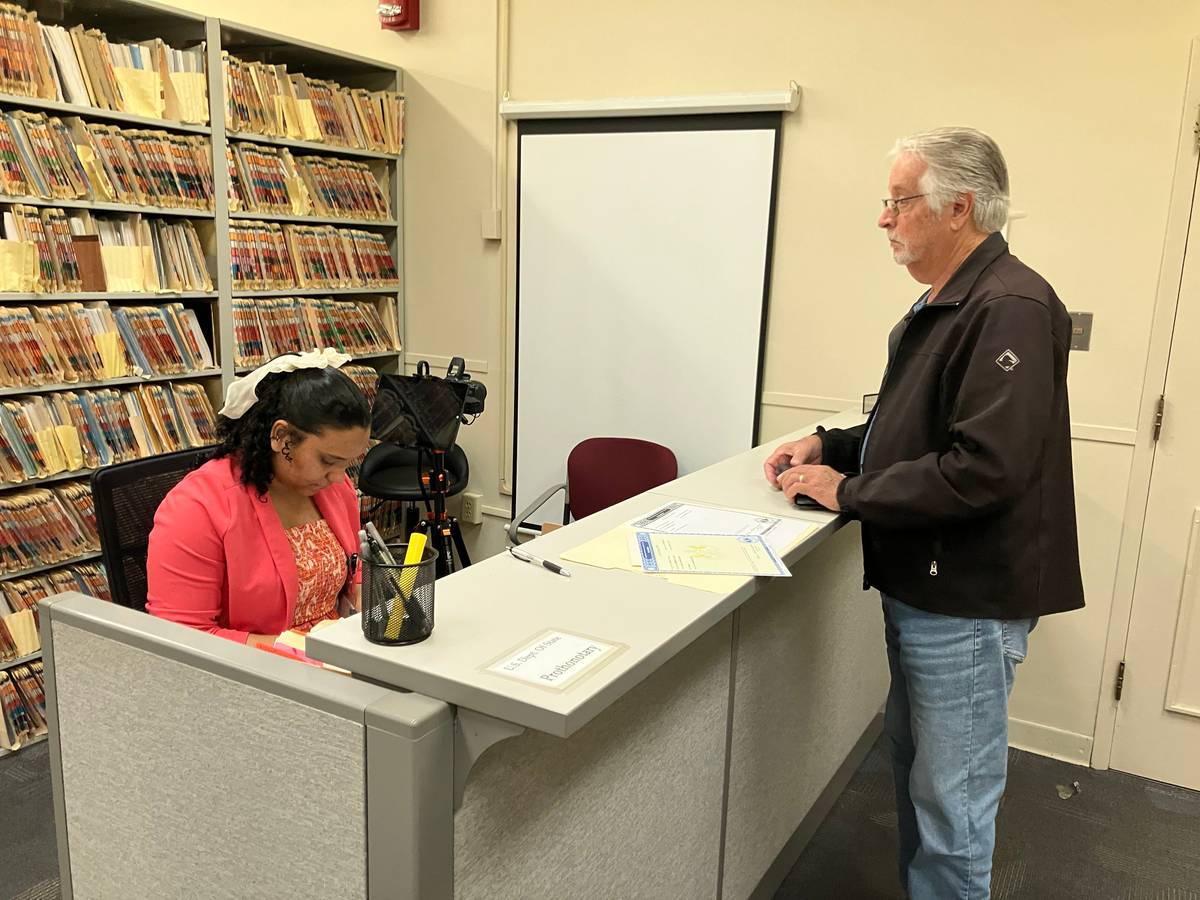
As part of the study, coroners’ offices in 67 counties were asked to complete surveys and participate in an interview. The researchers received full participation from 11 offices, and partial responses from 26. In north-central Pennsylvania, only the coroners’ offices in Mifflin and Lycoming counties fully participated. The coroners’ office in Blair County filled out the survey, while the coroners’ office in Clinton County allowed an interview.
Harry Holt, an associate professor in the Department of Health at West Chester University and another author of the study, said the researchers called and emailed each of the state’s coroners’ offices multiple times.
Centre County Coroner Scott Sayers, who serves on the executive board of the Pennsylvania State Coroners Association, said he didn’t participate in the study because he was busy.
“Nobody comes to our office to die,” Sayers said. “We have to go to them. Our work is out in the field — be it at a hospital, a residence, a roadway.”
Death investigations conducted by coroners can range from a review of medical records to a full autopsy and report. Autopsies, which involve surgically examining a corpse, require more qualifications than most coroners possess. They are usually outsourced to forensic pathologists, who are physicians with additional licensure and training to perform the procedure. Medical examiners also have the qualifications to perform them.
Coroners, particularly in rural communities, don’t have easy access to forensic pathologists, according to the study. Coroners have to rely on services for autopsies at labs that are sometimes hours away. Autopsies, VandePol said, are the gold standard for death investigations, but a lack of funding and personnel in some rural coroners’ offices disadvantage them relative to their urban counterparts.
That resource gap can prevent important details about a death from being determined. The National Association of Medical Examiners says autopsies should be performed for 13 categories, including deaths of children, deaths involving police, deaths that occur in the care of a local, state, or federal institution, and opioid overdoses.
Sayers said he works with a pathologist at Mount Nittany Medical Center, the local hospital, for autopsies. But when the pathologist there is away, his office works with pathologists in Johnstown or the Lehigh Valley. Sayers said his office performs autopsies for all overdose deaths, in case the district attorney wants to prosecute the person who distributed the drugs that caused the death.
Sullivan County Coroner Wendy Hastings, who also serves on the executive board of the state coroners association and participated in the study, said she is more selective about which autopsies her office performs.
“Sometimes things are cut and dry,” Hastings said, in the case of overdose deaths. If the county’s district attorney’s office is considering bringing charges against the person who distributed the drugs, it justifies an autopsy, she said.
Hastings said she supports the standardization of death investigations, but feels coroners’ offices should have the flexibility to investigate deaths based on the resources available to them.
The researchers conclude that more standardization and regulation are needed.
They recommend that all coroners’ or medical examiners’ offices have written operating procedures; stricter coroner qualification, certification, and training requirements; and that the state study how effective a more centralized medical examiner system would be.
They also advocate for incentives for people studying forensic pathology. The researchers suggest autopsy facility inspections, a set minimum number of morgue spaces, and more investment in forensic pathology facilities.
Hastings and Sayers agree that education would be more frequent and better if coroners were able to organize the training. Hastings said they would be able to do that if the Pennsylvania State Coroners’ Education Board that educates coroners — which is currently run by the attorney general’s office — were to operate under the Pennsylvania Commission on Crime and Delinquency.
That shift would allow the crime commission to manage the coroners’ association’s money, Hastings said.
Legislation that would place the education board operate under the Commission on Crime and Delinquency has passed the Senate and is pending in the House. Right now, the attorney general’s office receives the funding to facilitate the education of coroners through the Pennsylvania State Coroners’ Education Board.
One of the major barriers to additional training, VandePol said, is that many of the deputy coroners work part-time and have second jobs. Better funding would make full-time jobs at coroners’ offices more viable.
The Pennsylvania State Coroners Association is trying to increase the minimum yearly continuing education requirements from eight hours to 12 hours, or possibly even 16 hours, Sayers said.
But like so many things, it’s up to the state legislature to make changes.
Ashad Hajela is a Report for America corps member and writes about rural affairs for Spotlight PA’s State College regional bureau.
WHILE YOU’RE HERE… If you learned something from this story, pay it forward and become a member of Spotlight PA so someone else can in the future at spotlightpa.org/donate. Spotlight PA is funded by foundations and readers like you who are committed to accountability journalism that gets results.