This article is shared with LebTown by content partner Spotlight PA.
By Katie Meyer of Spotlight PA
HARRISBURG — Hundreds of thousands of Pennsylvanians could lose their health insurance and nearly two million could face more food insecurity in the coming months due to two sweeping rollbacks to pandemic-era federal policies.
Advocates see the sudden reduction of benefits as a looming health and welfare crisis. But they also view it as an opportunity to push the commonwealth, and its new Democratic administration, to do more.
The federal government will soon end a “continuous enrollment” policy that has kept states from kicking people off Medicaid for three years and stop sending extra monthly payments from the Supplemental Nutrition Assistance Program, or SNAP.
It’s a double whammy for people who rely on both programs. Cassie Hill is one of them. Her pay is inconsistent, so she’s not sure if, in the past three years, she edged above the income range that qualifies her for Medicaid. She also doesn’t know how she’ll make her grocery budget work when she’s getting less money from SNAP.
The 26-year-old North Philadelphia resident works as a dog walker and a clerk at a co-op, and her salary fluctuates significantly from week to week because her hours and the number of dogs she walks vary. A good month can bring in about $2,000. A bad one brings less.
She’s in recovery for an eating disorder, and the ability to use Medicaid to see a therapist consistently has been “life-changing,” she said. “It’s definitely not something I could afford if I had to pay for it.”
Likewise, SNAP has allowed Hill some peace of mind when it comes to food.
“I have a hard time being able to consistently make myself food,” said Hill, who also advocates for health care access with the volunteer group Put People First! Pennsylvania. “A huge part of my life is making sure that I have a lot of things that I can just grab and go. And food stamps have been indispensable for that.”
The changes to SNAP and Medicaid that have been in place since 2020 have had a big impact. Supplemental SNAP payments have given Pennsylvania households that use the program at least an extra $95 per month, often more. And in 2022, the uninsured rate in the U.S. hit an all-time low of 8%.
Now, the federal government is ending both measures.
In March, SNAP recipients will go back to getting one payment a month. That means nearly two million people in Pennsylvania will see their monthly allotments shrink by $181 a month on average, according to the state Department of Human Services.
And in April, people will need to resume reenrolling in Medicaid annually.
The department estimates that roughly 618,000 people will lose their Medicaid coverage because they no longer qualify for the program. It is keeping a separate list of 598,000 Medicaid recipients who haven’t resubmitted their annual paperwork over the past three years and are considered to be at higher risk of losing benefits due to logistical issues, even if they still qualify.
The impact on food security will be “big, like really big,” said Joe Arthur, who heads the Central Pennsylvania Food Bank.
Arthur said that in the 27 counties his organization serves, the value of the lost SNAP benefits will total more than $40 million when the extra payments end in March.
“To put that into some perspective, that is more food value than our entire network, and others, that provide food assistance would provide in a month,” Arthur said.
Nijmie Dzurinko who, like Hill, is an organizer with Put People First! Pennsylvania, said her group thinks the likely loss of health care benefits will be similarly significant. Her group views the situation “as a crisis,” she said.
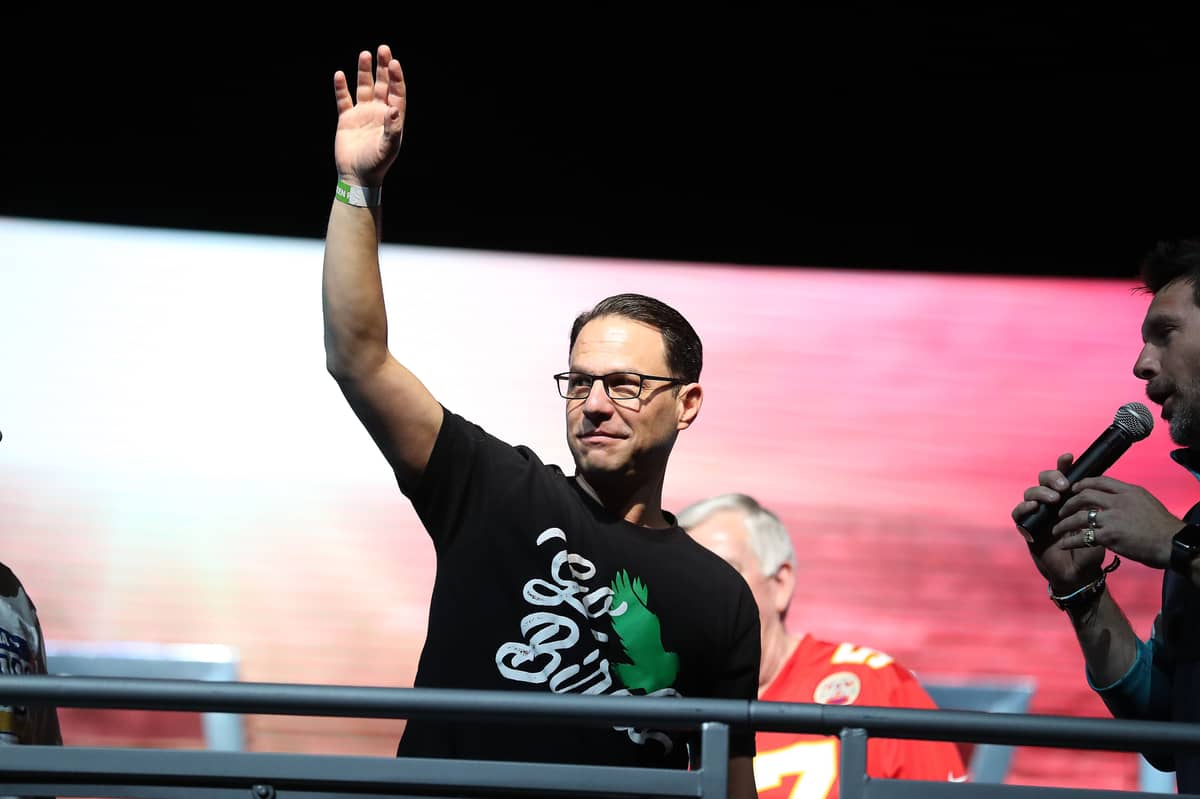
The Shapiro administration is primarily dealing with the rollbacks by trying to warn people about the changes to their benefits, and letting them know whether they have recourse under current law.
Over the past month, the administration has mailed letters to SNAP recipients warning them that February’s supplemental federal payment will be the last. Acting Department of Human Services Secretary Val Arkoosh is urging Pennsylvanians to donate to food pantries.
The administration is also reaching out to Medicaid recipients via “mail, text, email, and phone” to let them know they could lose coverage if they don’t reenroll in Medicaid beginning in April, DHS officials said in a statement. The date of expiration will depend on when a person’s Medicaid comes up for renewal; it happens annually at the date on which the person first got covered.
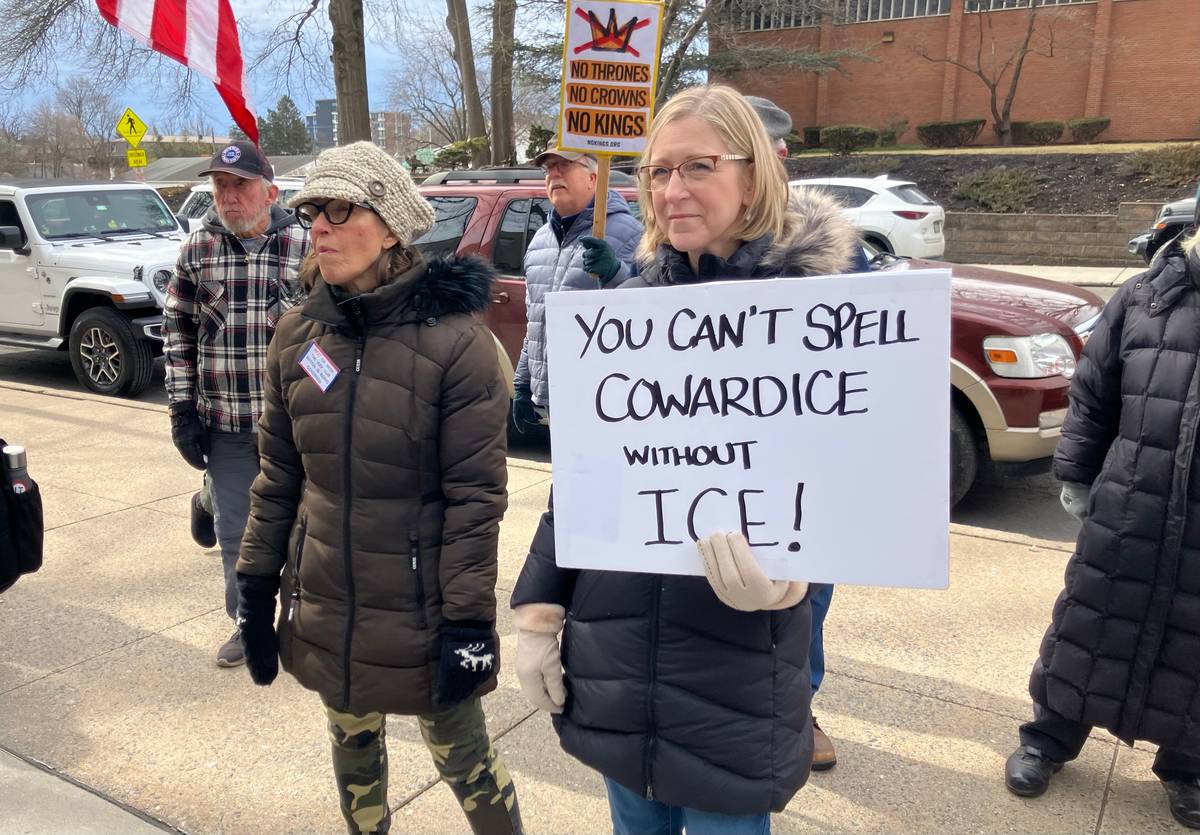
Advocates for guaranteed access to food and health care say they are concerned about the immediate impact on the people they work with. But they also see this rollback as an opportunity to push the administration to do more to take advantage of the existing opportunities states have to help people keep at least some of their benefits.
These include more quickly implementing a new federal requirement that would keep some from losing insurance coverage mid-year, passing legislation that would create state-funded food assistance payments, and exploring waiver options to further expand Medicaid.
“It shouldn’t just be kind of swept under the rug as ‘going back to normal,’” said Dzurinko. “It’s not actually a good normal that we had before.”

Stopping the churn
Health care advocates argue there is at least one concrete step the state can take right now to mitigate coverage losses.
One of the biggest problems that advocates for greater insurance coverage often point to in the Medicaid system is “churn” — people repeatedly cycling on and off the program due to paperwork problems or temporary changes in financial status.
Churn is an especially big problem for children, said Carolyn Myers of Pennsylvania Partnerships for Children, which advocates for expanded health care coverage. Myers argues that these past three years of continuous coverage solved a lot of that problem, but now that’s about to change.
“There’s been a 20% increase over those three years of children enrolled in Medicaid,” she said. “It supports healthy development at an early age.”
Of the Pennsylvanians projected to lose Medicaid coverage in the next year, Pennsylvania Partnerships for Children estimates about 430,000 will be minors.
Myers thinks there’s a way to reduce that number.
For years, the federal government has given states an option aimed at addressing churn in minors: They can choose to allow continuous 12-month coverage for kids, as opposed to kicking them off the program mid-year if, for instance, their families’ financial circumstances change.
Not all states have taken advantage of that option, though, Pennsylvania among them. The commonwealth currently guarantees 12-month continuous coverage for all children in the Children’s Health Insurance Program, or CHIP, but guarantees continuous coverage under Medicaid only for children 4 and under.
That will soon change. The federal appropriations measure that decoupled Medicaid and SNAP benefits from the COVID-19 public health emergency also turned that option into a requirement: States must provide yearlong continuous coverage for people up to age 18 who are enrolled in both Medicaid and CHIP beginning in January 2024.
But Myers doesn’t think the commonwealth should wait until then to expand 12-month Medicaid coverage to older children and minors.
“There’s no reason why we can’t implement this policy now,” she said. “There’s no hurdle.”
Pennsylvania Partnerships for Children is also urging Democratic Gov. Josh Shapiro to extend the continuous coverage provision to include people up to age 21.
Asked about the administration’s stance on those kinds of changes, Brandon Cwalina, a spokesperson for the Department of Human Services, said it “is open to exploring all options to improve the services we provide to Pennsylvanians,” though he didn’t offer more detail.

‘A political will conversation’
Advocates are also highlighting several legislative and administrative steps they’d like to see lawmakers attempt.
When it comes to food security, both Arthur of the Central Pennsylvania Food Bank and Ann Sanders, a policy advocate with the Pittsburgh anti-hunger group Just Harvest, said the commonwealth already uses most available federal resources.
Pennsylvania has “done a pretty good job,” Sanders said, but added, the governor and legislature could still take cues from other states on ways to further ease burdens and “help people adjust to having less benefits.”
Massachusetts, for instance, is considering putting extra money in its budget for additional months of supplemental SNAP payments. New Jersey is using state dollars to increase its minimum payment, and Maryland has a similar policy in place specifically for older adults.
Organizers with Put People First! Pennsylvania are also calling on the state to create an official public health care advocate. That position, also pitched in an unsuccessful bill last legislative session, would “hold … governments and the private sector more accountable,” Dzurinko said.
“We have an ombudsman for utilities and all these other things, but we don’t have that for health care,” she added.
People who work with SNAP and Medicaid recipients are also keeping an eye on the Department of Human Services’ staffing levels as it begins reenrolling people. Although the department sent out reenrollment paperwork over the past three years, the process was largely a formality rather than something that would make or break people’s health coverage.
“They have a lot of vacancies right now, especially clerical workers, which is really problematic when you talk about them having to renew three million Medicaid cases,” said Sanders.
She’s concerned, she said, that around May, “we’ll really start seeing people who are like, ‘I know I turned in my renewal packet. Why is my coverage getting cut off?’”
Myers of Pennsylvania Partnerships for Children is also watching how the state handles the logistically demanding reenrollment process.
“We really want DHS to do everything possible to protect Pennsylvania children from getting caught up in red tape and losing their health insurance,” she said. “And honestly, the administration has its work cut out for it.”
Cwalina said in a statement that the Department of Human Services will be able to handle the influx of work.
“DHS’ Office of Income Maintenance (OIM) will continue to monitor workloads across the County Assistance Offices (CAOs) and move work as necessary to other locations in an effort to ensure it is completed within established timelines,” he said in an email. “This is a typical process.”
Others are looking ahead to potential ways the state can even further reduce loss of coverage, taking inspiration from other states that are pioneering permanent multiyear continuous Medicaid coverage.
Last year, Oregon became the first state to give children continuous Medicaid coverage from birth to age six, and also instituted two-year continuous coverage for children and adults six and older.
The state did this using a federal waiver that is designed to test new approaches to Medicaid coverage to see if they improve outcomes. If approved by the federal Department of Health and Human Services, these waivers often authorize new programs on a five-year basis, and require among other things that they not cost the federal government additional money.
Three other states — California, New Mexico, and Washington — are now pursuing similar waivers.
Elisabeth Burak, a senior fellow with the Georgetown University Center for Children and Families, said pandemic-era continuous enrollment has already given states an unusual opportunity to track the impact the change can make. In her opinion, that evidence has been compelling.
States like Oregon, she said, “saw the uninsurance rate drop for kids of color, you know, significantly, because they didn’t get disenrolled and come back on.”
“I do think it’s a common sense way to make sure your kids are staying on and they can get the care they need instead of, you know, having to deal with the added stress of coverage gap,” she said. “I think it’s going to be a political will conversation.”
Cwalina said the Shapiro administration is “open” to these measures, adding, “some of these changes would require federal or state legislative action and DHS stands ready to work with our respective delegations to consider additional ideas.”
WHILE YOU’RE HERE… If you learned something from this story, pay it forward and become a member of Spotlight PA so someone else can in the future at spotlightpa.org/donate. Spotlight PA is funded by foundations and readers like you who are committed to accountability journalism that gets results.