A former ELCO girl’s basketball great was living a good, vibrant life in South Florida with her husband and their two young sons when Parkinson’s disease began a slow but steady advance that would change their lives forever.
It’s a reality Dane and Alicia Hartlaub Ireson have been dealing with since a surprise diagnosis in 2020.
Though it can still cause great discomfort and significant emotional and physical distress while eventually completely disabling those afflicted by it, Parkinson’s disease, thanks to the marvels of modern technology and medicine, is not quite as devastating as it used to be.
Unless, of course, yours is the life it’s disrupting and your family is the one that is burdened with taking care of you and sharing in your struggles while also trying to keep their own lives on track. Then, the general acknowledgement from the medical community that Parkinson’s, an incurable disease, has evolved into a treatable and livable condition isn’t quite as comforting.
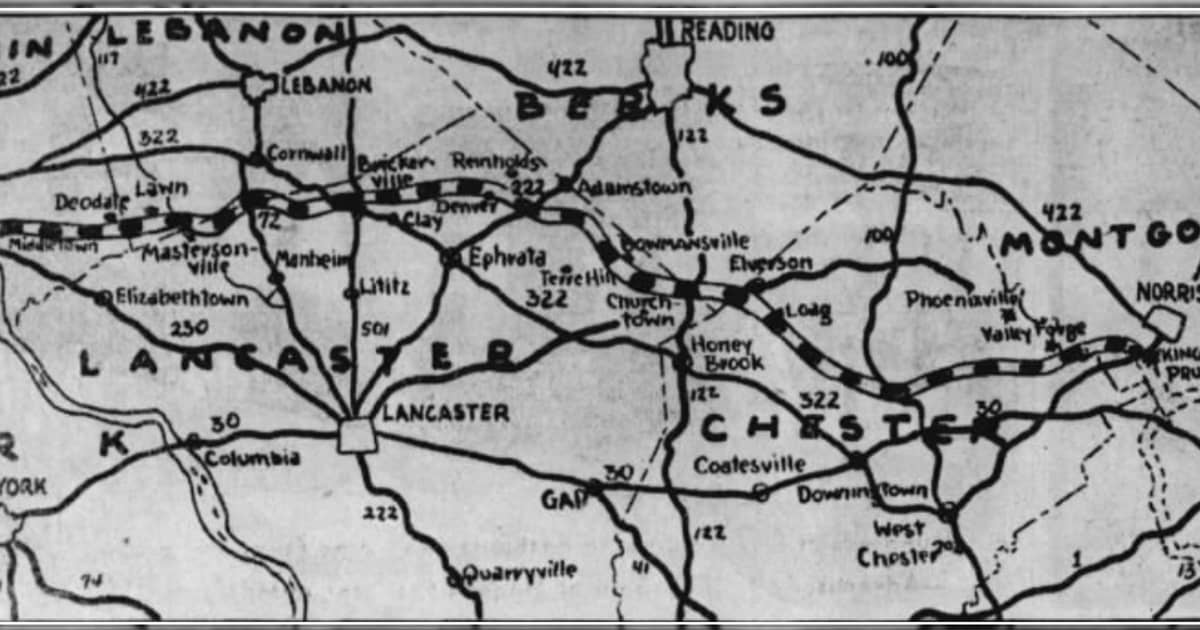
Like the rest of the world in late 2020, which was dealing with the COVID-19 pandemic, the Iresons had their share of headaches, but life in general was still pretty good. Married since 2014, the two former athletes — Alicia starred as a power forward on some imposing late ’90s ELCO girl’s basketball teams and later turned in a solid college hoops career at the University of Miami, while Dane, an Elverson native, was a standout linebacker/defensive end at Florida International — had settled into careers as special education teachers and coaches in the Palm Beach County School District. They started a family and were raising two young boys in the South Florida sun.
And then their world turned upside down. In October 2020, Dane, then 38 years old, received the bad news.

“I was in my early 40s, with a lot of life before me, when a moment came and stopped me on a dime. I spent most of the next days looking at the X-rays, talking about the options, and talking about sweet time.”
The lyrics from Tim McGraw’s hit song, “Live Like You Were Dying,” listed above did not apply 100 percent to Dane, thankfully, but the impact of hearing the words “— “Parkinson’s disease” —” felt all too similar to McGraw’s song.
Compounding the problem was needing a diagnosis during COVID when resources were already stretched to the limit and the non-motor aspects of Parkinson’s were sneaking up on him.
“I was so strung out by anxiety and depression,” Dane said of that time.
He was also dealing with what he thought was shoulder stiffness, something that many Parkinson’s patients report as one of their earliest symptoms. Still, he wasn’t exactly prepared for what he heard after he finally saw a neurologist.
“He looked at me, and said, ‘I know what’s wrong with you,'” Dane recalls. “I said, ‘What?’ He said, ‘You have Parkinson’s.’ In my mind, I didn’t accept that. He told me that I’d have to take medication, and I said, ‘I just take a pill, and it’ll go away, right? Because I don’t have it.’ He said, ‘No, you have to understand.'”
Dane’s skepticism was understandable, given that the majority of people diagnosed with Parkinson’s are around age 60, the average age of onset. But 5 to 10 percent of patients are classified as “young onset,” diagnosed under the age of 50. It was not a club he was looking to join.
“It humbles you,” he said. “You have to ask for help more, you have to rely on people more, you have to be more vulnerable with people.”
He also had to get used to the fact that taking medication and taking it on time was now a part of his daily life.
The good news is the main Parkinson’s drug, carbidopa levodopa, is usually highly effective and can often bring about significant improvements in the early stages of the disease. Eventually, though, the meds begin to lose some of their effectiveness, and side effects become more prevalent.
“Four-hour increments,” Dane said of the time period between doses. “If they work, it’s great. Sometimes, a dose will misfire and won’t work. And If they don’t work, you don’t work.”
Fortunately for Parkinson’s patients like Dane, today there is a new weapon with which they can fight back against some of the more debilitating aspects of the disease — deep brain stimulation surgery, or DBS.
Approved in 2002, DBS has become an accepted treatment for Parkinson’s in recent years and can have a huge impact on a patient’s condition, often allowing for significant medication reductions, improving motor function, and reducing symptoms in 85 to 89 percent of patients.
How does it work? A surgeon implants electrodes in the brain areas that control movements and they are attached to a battery-operated neurostimulator implanted in the upper chest that is controlled by a computer.
It is not a cure and does not halt the underlying progression. Like any surgery, there is the possibility of infection and complications, and quite frankly it’s not for everyone because, well, it is brain surgery.
But it can restore some quality of life, and in July 2023, Dane underwent DBS. It hasn’t fixed everything, but it has given Alicia her husband – and their kids their fun-loving dad – back. And it has allowed Dane to continue teaching while also seeing his wife every day since she teaches in the same building.

“I would say that pre-DBS, Dane was really like a zombie,” Alicia said. “Not very involved. Not participating in life, he wasn’t able to. Post-DBS, even my 6-year-old would say that dad jokes more. I think DBS did help him. His personality came back; his humor returned.”
“I feel like I can do more, I can do more with the kids,” Dane said, although he still battles significant Parkinson’s-related fatigue. “I feel more like a person.”
It still takes work though, most notably the DBS programming he must periodically receive in order to keep the symptoms at bay. Good programming, normally done by a neurologist experienced in movement disorders like Parkinson’s, is absolutely essential to a patient’s quality of life. If that is not done, satisfaction with the surgery can plummet.
But when it’s good, it’s really good.
“For like a week after programming, I’m on cloud 9,” Dane said.
And if the DBS procedure continues to be refined and improved, he could be looking at more than the 10 to 15 years of benefit that Parkinson’s patients currently receive.
“It’s been a journey, I’ll say that,” said Alicia, who serves as Dane’s caregiver. “Normally, it’s a moment-to-moment disease for him. There’s times when I have to explain to the kids that dad’s gonna have to sit this one out.”

The reality is that unless a cure is found or DBS is able to stop the progression, Dane’s condition will not magically get better.
So the Iresons will enjoy what they can when they can and live life in the moment.
Because reality isn’t going away anytime soon. They don’t necessarily like that. But they accept it, and do what they must to still have great experiences like planning family vacations.
Venting is also encouraged.
“It’s such a shitty disease,” Alicia said, accurately summing it all up quite nicely. “That’s what it is. It’s just a shitty disease.”
Questions about this story? Suggestions for a future LebTown article? Reach our newsroom using this contact form and we’ll do our best to get back to you.

Keep local news strong.
Cancel anytime.
Monthly Subscription
🌟 Annual Subscription
- Still no paywall!
- Fewer ads
- Exclusive events and emails
- All monthly benefits
- Most popular option
- Make a bigger impact
Already a member? Log in here to hide these messages
An informed community is a stronger community. LebTown covers the local government meetings, breaking news, and community stories that shape Lebanon County’s future. Help us expand our coverage by becoming a monthly or annual member, or support our work with a one-time contribution. Cancel anytime.