What current statistics are showing about the COVID-19 pandemic is that fewer people are getting sick, fewer people are being hospitalized and fewer people are dying. Since vaccines were made widely available about two months ago, the number of new COVID-19 cases, the number of people hospitalized with the coronavirus and the number of deaths related to the virus have all been on the decline.
WellSpan Health System operates seven hospitals in the south-central Pennsylvania region, including the Good Samaritan Hospital in Lebanon.

“In the fight against COVID-19, vaccines are the single most important thing we do,” said Dr. Tony Aquilina, WellSpan Health’s executive vice president and chief physician executive. “Our treatment is generally supportive, but the best way to do it is to prevent it. The two vaccines we use – the Moderna vaccine and the Pfizer vaccine – have been incredibly effective and remarkably safe.”
“Some people have had side effects,” continued Aquilina. “But the rate at which they have kept people out of the hospital is almost 100 percent. If the virus doesn’t spread, it can’t create a variant. If the virus isn’t spreading, it’s not mutating.”
In April, the first full month that vaccines were offered to the general public locally, 476 patients exhibiting COVID-19 symptoms were admitted to WellSpan’s seven hospitals, and of that number, only seven had received both doses of the coronavirus vaccine. Put another way, 469 of the COVID-19 patients who were admitted were not vaccinated.

“When I look at statistics, I look at the sheer number of new (Covid-19 cases),” said Aquilina. “I know a certain percentage of those will be admitted to our hospitals. I also look at the transmission rate, and when I do, I’d like to see that be less than five percent. Most of the state is less than five percent. We also look at the mortality rate of people who are in the hospital, and the current mortality rate is down to nine percent. That means, on the average, of 100 people who have been admitted with COVID-19, 91 people leave our hospitals alive. But that’s still a lot of people dying.”
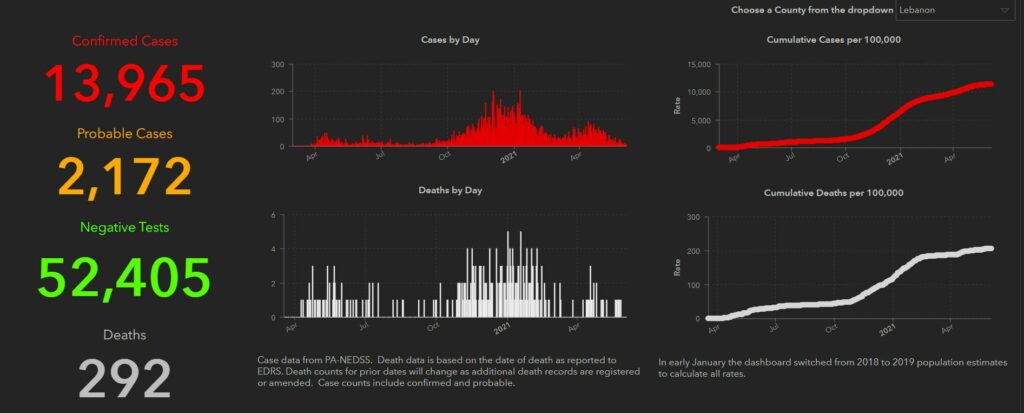
“Lebanon County’s numbers have gone up and down, like everybody else’s,” added Aquilina. “The good news is that they’re down right now.”
According to the Pennsylvania Department of Health, there were 33 confirmed cases of the Coronavirus during the week of May 28 to June 3 in Lebanon County, some 43 less than there were in the week before. Throughout the state, the total number of COVID-19 cases were down by 2,108 during the week of May 28 to June 3, compared to the last full week in May.
“We’re reliant on the state,” said Aquilina. “I can tell you that the state is saying that we’re approaching a 70 percent vaccination rate for our adult population, and that it’s good to take off our masks. We know that in some of our south-central counties, we’re not at that level. Currently, 55 percent of the total population across the state has received both doses.”
“There are fears because (the vaccine is) new,” Aquilina added. “When we look at our employees’ concerns about the safety of our vaccinations, it’s because it’s new.”
The average age of people hospitalized for COVID-19 throughout the WellSpan Health System is 66.4 years. To this point, a total of 134 local residents have died of complications related to the coronavirus at the Good Samaritan Hospital.

“Data is critically important,” said Aquilina. “It’s how you learn and understand. You’ve got to take the politics out of it. The truth is in the data. It’s a very serious illness. Given how infectious it is, we have to stop it. Our data shows that virtually no patients who have been vaccinated have been admitted to our hospitals for the last two months.”
“This is a really infectious virus to everybody,” Aquilina continued. “It makes you sick, and it doesn’t matter how healthy you are. We spread it around every easily. The new cases we’re seeing now are in younger people.”
Much like the world and the rest of the United States, Lebanon County has tried to control and manage the COVID-19 crisis to the best of its ability. Locally, the severity of the pandemic was first fully realized in March of 2020, and it was met with mitigating efforts that included face masks, social distancing and an increased awareness of washing hands.

“COVID-19 started a little before March. We started worrying about it in January and February (of 2020),” said Aquilina. “We knew very little about it. It spread rapidly in the United States. In April, we had a lock down across the world to reduce the number of cases. The lock down helped us figure out what to do next. During the fall, it came back, and in the winter, it was stronger than ever. We actually had four surges in Pennsylvania.”
“It’s not over,” continued Aquilina. “We still have 60 people in our hospitals who have COVID-19. That’s much lower than the peak, and that’s much lower than a month ago. It’s great news, and most of it is because of vaccines. It is certainly a safer situation compared to a month ago or over the winter. When will it be over? The answer is when we get to herd immunity. But we will get back to normal.”
The effectiveness of the world’s response to the COVID-19 pandemic will be debated by scholars for years to come. But what’s important to remember are the lessons that have been learned throughout the process.
“We are getting more data every day,” said Aquilina. “We have to remember that it’s not a political issue. It’s an issue of health and safety. It has become crystal clear that the way to combat COVID-19 is through vaccinations.”
“Smallpox was way worse than COVID-19, just for the sheer number of people it killed indiscriminately,” concluded Aquilina. “Now, there are no clinical smallpox cases in the world, and it’s because of vaccines. The way to wipe out something like this is with vaccines. I think we’ll get to that point in the United States. The question is if we’ll be able to get to that point in the world.”